By Amanda Linneman RN, BSN
Clinical Team Manager
Consure Medical
Incontinence is the inability of the body to control the evacuative functions of urination or defecation, a partial or complete loss of bladder or bowel control. To me, incontinence is so much more.
Incontinence is embarrassment, shame, the fear of sneezing or laughing aloud in public. It is always having to have the bathroom close by, an extra change of clothes in the car. Can you imagine living with this condition for a few weeks (eg. Post partum incontinence) to few years (eg. Urge incontinence in Geriatric patients).
I spent a good portion of my professional life in the Burns Unit of major US hospital systems. Third degree, fourth degree, pediatric pranks, young adults involved in accidents, industrial fire and injuries – I have seen it all. A common thread in most of these patients was incontinence.
To me, and thousands of nurses like me, incontinence is frustrating. It means ‘lotions and potions’ for my patients, multiple bed linen changes and patient baths, diapers to change, yeast and pillow cases in skin folds, an inaccurate urine output measurement. It means more time needing to be spent in the patient room, the need for additional patient care staff in the middle of a nursing shortage. It means potentially Incontinence Associated Dermatitis (IAD) a potential hospital acquired pressure injury (HAPI), a potential foley catheter, condom catheter, external urine management device, inflatable balloon catheter (IBC), rectal pouch or rectal tube, a potential Catheter Associated Urinary Tract Infection (CAUTI) or injury. It means time, money and potential hospital fines from incontinence related injury if incontinence is not managed appropriately.
Incontinence is a lot more than people give it credit for. It usually presents in a benign form, almost always a Secondary clinical condition (patients rarely get admitted to ICU for Incontinence), and creates havoc in care facilities world-wide.
Incontinence impacts 100 million patients each year and costs more than $10 Billion in treatment/management costs [Ref: 1]. Around 13 million people in the U.S. present with incontinence each year [Ref: 2]. While older age increases the risk of this condition, there are a wide range of factors that can cause this problem in younger persons – eg. Smoking, obesity, diabetes mellitus, spinal cord injury, substance abuse, etc . Meanwhile, women are much more likely than men to experience incontinence mainly due to weakness of the ano-rectal apparatus due to child-birth. Menopause. etc. Both women and men can become incontinent from neurologic injury, congenital defects, strokes, multiple sclerosis, and physical problems associated with aging.
Table 1: Incidence & Prevalence of Urine Incontinence in US Hospitals
| HOSPITALS | Nursing Home | Hospice | Residential Care | Home Agency | ||
| Critical Care Units | Emergency Departments | |||||
| # Of Centers | 6146[Ref: 3] | 6146[Ref: 3] | 15,600[Ref: 4] | 4,000[Ref: 5] | 30,200[Ref: 6] | 12,400[Ref: 7] |
| Prevalence | 45-79%[Ref: 8] | 2.8%[Ref: 9] | 50-65%[Ref: 10] | 24%[Ref: 11] | 42-50%[Ref: 12] | 40.2%[Ref: 13] |
| # Of Patients | 4.3M | 4.9M | 0.9M | 0.3M | 0.4M | 0.5M |
Table 2: Incidence & Prevalence of Fecal Incontinence in US Hospitals
| Critical Care Unit | Nursing Home | Hospice | Residential Care | Home Agency | |
| # Of Centers | 6146[Ref: 3] | 15600[Ref: 4] | 4,300[Ref: 5] | 28,900[Ref: 6] | 12,200[Ref: 7] |
| Prevalence | 9-40%[Ref: 14] | 42-50%[Ref: 15] | 24%[Ref: 16] | 42-50%[Ref: 17] | 9.7-12%[Ref: 18] |
| # Of Patients | 2.3M | 0.7M | 0.3M | 0.4M | 0.6M |
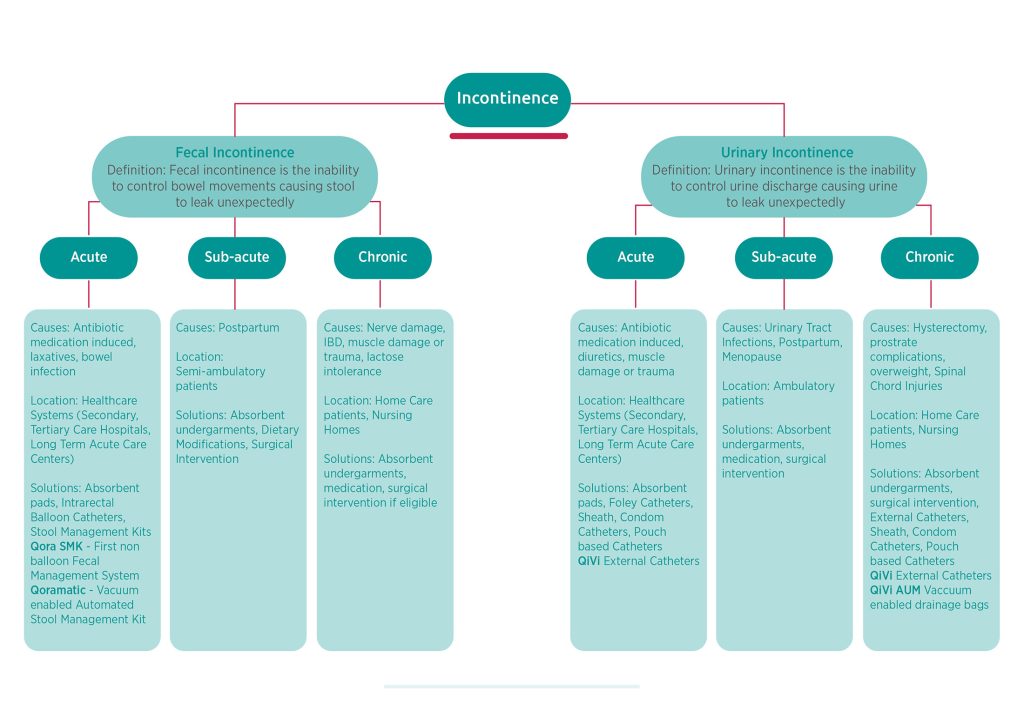
Figure 1: Clinical Definitions and Presentation
Overview of available Incontinence Management solutions
While I empathize with patients suffering from short term incontinence related to child birth, menopause or prostate, as well patient suffering from long-term/permanent incontinence, the biggest cost of incontinence is in the hospitals.
There are over Five Million admissions in ICUs each year [Ref: 19]. Over 50% of these patients suffer from at least one form on Incontinence (See table 1 & 2). Complications arises when the acid mantle of the peri genital skin starts to break down causing diaper-rash or a more adult friendly nomenclature – ‘perineal rash’. Sebum, an oily substance secreted, through the sebaceous glands maintains the skin integrity and maintaining an acidic pH of 4 – 6.8. Feces containing protease and lipase, both alkaline in nature, can digest perianal skin and soft-tissue. These pathological manifestations combined with physical forces of patient weight, skin friction from restlessness and agitation of patients, leads to further skin breakdown. In patients with double incontinence, the moisture of the urine causes over-hydration of the skin and the urea and ammonia present in the breakdown of urine lead to an alkaline pH, which is further exacerbated by fecal urease. These combine to adversely impact the acid mantle, exposing the skin to bacteria and other microorganisms. Studies have shown that skin permeability is compromised after 2 or more days of prolonged exposure to water. Urine and feces start to damage the skin in a much shorter time. Ongoing exposure to moisture from fecal incontinence causes the skin to macerate, thus compromising the skins integrity as a barrier.
Unattended or untreated macerated skin results in erythema, and pain over a period of time. Skin with an impaired barrier function can easily be invaded by bacteria causing acute dermatitis. Instead of calling it ‘rash’, the medical community, since 2007, has adopted a new terminology for this condition called ‘incontinence associated dermatitis’ (IAD). IAD is defined as skin inflammation manifested as redness with or without blistering, erosion or loss of skin barrier function that occurs as a consequence of the chronic or repeated exposure of the skin to urine or fecal matter”.
In hospitals, we spend millions on dollars per year in patient surfaces to manage pressure injuries (ulcers is no longer the preferred nomenclature). However, pressure injuries start due to weight of the patient, friction/shear of the skin surfaces and weakness or damage to the skin surface caused by wetness. An incontinent person is 22 times more likely to have pressure injuries [Ref: 20]. These pressure injuries most often initiate in the ICU and hence term HAPI – Hospital Acquired Pressure Injury.
In addition to incontinence associated dermatitis (IAD), HAPI, incontinent patients are also at risk for secondary infections like urinary tract infections (UTI), blood stream infections (BSI), and the most expensive nosocomial infection called Clostridium difficile (C-Diff).
The cost of these complications and infections is huge. Catheter Associated Urinary Tract Infection (CAUTI) costs $10,197 [Ref: 21], C.Difficle infection cost is $29,000 [Ref: 22], Surgical Site infection is $34,434 [Ref: 23], and Pressure injuries cost anywhere between $ 14,839 – $21,410 [Ref: 24].
Fecal and Urine incontinence may lead to complications that increase the length of stay of a patient by 5-7 days, which results in additional $20,000 – 30,000 in spend per patient. More importantly, the Mortality of an incontinent patient goes up 7% due to the above-mentioned complications.
Again, incontinence is almost never the primary condition of the patient. They get admitted in the ICU for trauma, stroke, post-surgery, and in my case for severe burns, yet ends up costing our healthcare system close to $ 10 Billion per year in direct and in-direct costs.
Nurses spend close to 170 minutes per day in toileting and dressing the patient [Ref: 25], and incontinence is a major source of back injuries, fatigue, demotivation and attrition.
I personally believe in 2022 we still do not have the best tools to manage and treat incontinence. Like most nurses, I consider myself to be quite industrious and innovative. I am now the Clinical Program Manager for a nurse centric company with a sole focus on design, development and commercialization of Incontinence management products. (Consure Medical – www.consuremedical.com)
In a future blog post, I will provide an overview of available clinical solutions, latest innovations and a sneak preview on where we are headed. Stay tuned!
References –
- 2001_Wilson_Annual Direct Cost of Urinary Incontinence
- Managing acute and chronic urinary incontinence. AHCPR Urinary Incontinence in Adults Guideline Update Panel. Am Fam Physician.
- https://www.aha.org/statistics/fast-facts-us-hospitals
- https://www.cdc.gov/nchs/fastats/nursing-home-care.htm
- https://www.cdc.gov/nchs/fastats/hospice-care.htm
- https://www.cdc.gov/nchs/fastats/residential-care-communities.htm
- https://www.cdc.gov/nchs/fastats/home-health-care.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114799/
- Schuur, et al. Urinary Catheter Use and Appropriateness in U.S. Emergency Departments, 1995–2010
- 2018_Felix_UI Prevalence in Nursing Homes
- 2017_Shackley_UC Prevalence in Hospitals
- Felix et al., Urinary and Fecal Incontinence in Nursing Home Residents.
- https://www.cdc.gov/nchs/data/series/sr_03/sr03_036.pdf
- Bayon Garcia, Intensive Care Society, 2013
- Saga et al., BMC Gerioatrics, 2013
- https://www.cdc.gov/nchs/data/series/sr_03/sr03_038.pdf
- https://www.cdc.gov/nchs/data/series/sr_03/sr03_038.pdf
- Halland et al, Dis Colon Rectum. 2013
- http://www.sccm.org/Communications/Pages/CriticalCareStats.aspx
- Maklebust J, Magnan MA. Risk factors associated with having a pressure ulcer: a secondary data analysis. Adv Wound Care. 1994;7(6):25 -34
- Stone PW, Economic Burden of healthcare-associated infections: an American perspective. Expert Rev Pharmacoecon Outcomes Res. 2009;9(5):417-422.
- Lipp MJ, et al., Impact of hospital-acquired Clostridium difficile.. Journal of Gastroenterology and Hepatology 2012;27(11):1733-1737
- Shepard J, Ward W, Milstone A. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surg. 2013 Oct;148(10):907-14.
- Spetz J, Aydin C, Brown DS, et al. The value of reducing hospital-acquired pressure ulcer prevalence: an illustrative analysis. JONA. 2013; 43(4): 235-241.
- Data on company file

